THERE ARE OVER 30 MENOPAUSE SYMPTOMS
Some are well known like hot flushes and weight gain, others are unusual like a burning mouth or dizzy spells.
Scroll down to find symptom information.
For personalised recommendations to resolve your symptoms, see our testing packages and Lose Weight plan.
If you have any specific questions, book a free 30 minute call with one of our menopause experts.
MOST FREQUENTLY SEARCHED SYMPTOMS:
Lots of menopausal women put on weight or find it much harder to lose weight despite exercising harder and eating less. In fact, one study revealed that the average woman puts on 0.5kg per year from their mid 40s.
Menopausal weight gain is different from the weight gain you experienced when you were younger. It’s about an imbalance in ‘hunger hormones’ and a shift that that means you are more likely store food as fat.
Many women struggle with insulin resistance which is compounded by stress which also interferes with blood sugar. These encourage fat to be stored around the stomach, in particular.
Other factors include reduced muscle mass (muscles burn calories, even at rest), a slow thyroid impacting your metabolic rate and, last but not least, poor sleep.
Weight loss is much easier when your diet and supplements are focused on rebalancing your hunger hormones and managing cravings alongside doing the right type of exercise, improving how your body responds to stress and getting good quality sleep.
If you are frustrated and feeling self-conscious about weight you can’t shift, no matter what you try, check out our Lose Weight programme. We will create you a personalised plan that enables you to lose menopausal weight without feeling hungry and deprived.
Anxiety is very common during menopause. It can creep up slowly or hit you suddenly and leaves you feeling fearful, tense and overwhelmed. Physical symptoms associated with anxiety include an elevated heart rate, heart palpations, shaking, chest pains, sweating and feelings of nausea. At its extreme, anxiety can become a panic attack.
There are many causes of menopausal anxiety. One is the link between oestrogen levels and serotonin, another is that between progesterone and GABA (which calms the brain reducing overthinking and worry). Too much cortisol can make us anxious too.
One very simple tip, which can be done anywhere, is to use your breath to calm you down. Aim to breathe very slowly in and out and you’ll feel your system slow.
You are not alone if you feel drained and zapped of energy during the menopause – both physically and mentally.
During menopause, our hormone levels fluctuate dramatically which can disrupt sleep and leave us tossing and turning at night and waking up feeling unrefreshed.
Where insulin sensitivity is an issue, our cells don’t receive sufficient fuel from the food we eat which takes away our get-up-and-go. Thyroid issues, low iron levels and low B vitamins can also reduce energy levels
When we’re tired, we’re less likely to do exercise but this can set up a vicious circle as doing exercise boosts our energy.
Please note there are also medical conditions which can result in fatigue such as pain, sleep apnoea and infections – please discuss these with your doctor if you think they apply to you.

ALL THE SYMPTOMS:
Muscle aches, pains and stiffness are reported by many women through menopause.
Muscle tension can be caused by a number of hormonal changes.
Starting with the sex hormones – lower levels of testosterone can impact the body’s ability to build muscle and therefore result in muscle weakness and fatigue. Reduced progesterone levels impact the amount of muscle relaxing neurotransmitters in our brain which can leave your muscles feeling tight.
Your thyroid could also be a factor – a slow thyroid can cause muscle aches and tenderness.
Watch out for poor posture and spending too much time sitting down. Prioritise exercise that supports muscle growth and flexibility.
As well as hot flushes, broken sleep and mood swings, the menopause can also see a worsening in allergies or even see new ones develop.
Changing oestrogen and progesterone levels can increase some women’s sensitivity to histamine levels.
This can make you more sensitive to allergens than normal and there are certain ‘high histamine’ foods which are best avoided. If this is you, avoid eating too many aged foods such as wine and cheese and fermented foods such as sauerkraut and kimchi.
Anxiety is very common during menopause. It can creep up slowly or hit you suddenly and leaves you feeling fearful, tense and overwhelmed. Physical symptoms associated with anxiety include an elevated heart rate, heart palpations, shaking, chest pains, sweating and feelings of nausea. At its extreme, anxiety can become a panic attack.
There are many causes of menopausal anxiety. One is the link between oestrogen levels and serotonin, another is that between progesterone and GABA (which calms the brain reducing overthinking and worry). Too much cortisol can make us anxious too.
One very simple tip, which can be done anywhere, is to use your breath to calm you down. Aim to breathe very slowly in and out and you’ll feel your system slow.
Fluctuating hormones during menopause can cause uncomfortable bloating for some women.
At the beginning of perimenopause, when our oestrogen levels are high and progesterone begins to drop, we can experience water retention which again makes us feel bloated.
As oestrogen levels then drop, our digestion can become sluggish which increases transit time and increases bloating and constipation.
Low thyroid hormones and insulin resistance also cause fluid retention.
Some women also find they have more gas as their gut bacterial balance changes through menopause.
Often described as feeling your brain has turned into cottonwool. Brain fog means it can become tricky to concentrate, maintain your train of thought or find the right words and names. However it affects you, it’s frustrating and can be embarrassing.
Brain fog is very common – estimates range from 40% to 73% of menopausal women.
Whilst oestrogen plays a role, the real culprit is brain cells not being able to produce enough energy.
The right diet and exercise choices that support improved insulin sensitivity and blood sugar balance can get you back to being sharp witted.

Your nails are made up of layers of a protein called keratin, produced in the nail bed. It is normally hardwearing.
However, as oestrogen levels drop it can dehydrate which makes it weaker, more prone to breakage and harder to grow.
Other factors include an under-functioning thyroid, insufficient protein in the diet and low levels of iron.
Don’t overlook the damage we ourselves can do to our nails – acetone nail remover is harsh and drying, false nails are not kind to your actual nail.

Yes, your sweat may well smell different and it’s linked to the menopause.
There are 2 elements here.
Firstly, more sweat. Thanks to lower levels of oestrogen, our thermostat becomes tighter which means our bodies start sweating at lower temperatures to try to cool down. We can also sweat more due to anxiety and stress, both common through menopause.
Secondly, more potent sweat. Our apocrine sweat glands (e.g. in our armpits) are impacted by the relatively high levels of androgens vs oestrogen which leads to more bacteria and the chance of stronger smelling B.O.

Post adolescence, the female silhouette has a defined waist. As we transition through perimenopause and menopause, however, it is common to disproportionately put on weight around our mid-line which means we can lose our waist.
This is due to changing levels of hormones (oestrogen insulin and cortisol) and a tendency to put on weight around our stomachs instead of bottom and thighs.
Goodbye pear, hello apple.

As sex hormone levels change and become erratic, your menstrual cycle is likely to be knocked off course. If your period used to be regular, chances are that’ll no longer be the case.
This is one of the most noticeable early signs of perimenopause (although not if you are on hormonal contraceptive).
We are all different so your menstrual cycle changes will be unique – it may become heavier or lighter, longer or shorter.
As you progress through perimenopause, your periods will eventually stop. When you have not had a period for 1 year you have hit menopause and beyond that you are post-menopausal.
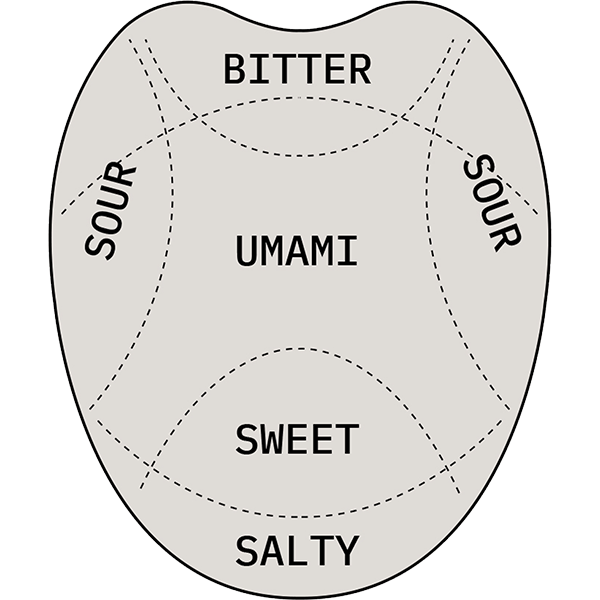
How intensely we smell and taste changes as we age and this accelerates for some women through menopause.
Lower levels of oestrogen reduce saliva which in turn affects our taste sensation. Saliva does an important job breaking down food into individual chemicals which are then picked up by our taste buds. Put simply – a dry mouth tastes less.
However this is not the only cause, low zinc levels and sinus infections can reduce or change taste.
Some women experience strange or unpleasant tastes (such as metallic, bitter or salty) even when they aren’t eating.
A good start point is to stay hydrated and avoid food and drinks that dehydrate you (such as anything very hot and spicy, alcohol and caffeine).
Digestive issues can rear their head through menopause. Indigestion, acid reflux, bloating, abdominal cramps, diarrhoea, constipation, flatulence and nausea can be common.
There can be many causes for digestive problems. Lower levels of oestrogen slows the rate food passes through the gastrointestinal tract. If you already have IBS (Irritable Bowel Syndrome) you may find it gets worse through menopause.
Chronic stress can impact the effectiveness of your digestive system (causing diarrhoea, wind and bloating) as can the diversity of your gut bacteria, known as your microbiome. Stomach acid need zinc to be optimised.
Feeling dizzy, light-headed, a little ‘faint’ or like the room is spinning around can occur at menopause.
A key factor is blood sugar levels – when they become erratic (high or low), it can make us feel dizzy. Stress, being under-slept, anxiety, dehydration, hot flushes, headaches, low blood pressure – they all too can play a part.
Low iron, as a result of heavy bleeding, is also a factor.
Aim to eat well to stabilise your blood sugar.
Finally, some women, after a sustained period of stress, have low cortisol levels which can lower blood pressure and make you feel dizzy and faint.

The ageing of our skin is inevitable but you’re not going mad if it seems to accelerate through perimenopause and menopause.
As oestrogen levels decline, the amount of collagen in our skin also declines which makes it thinner. At the same time, lower levels of progesterone contribute to drier skin (with less sebum being produced). This combination can result in wrinkles, sagging and crepiness.
Our lifestyle choices are important too, it’s just not about hormones. UV damage is a key factor, as is smoking. Choose healthy fats, eat protein and stay hydrated to help out your skin.
Some women experience a short, sharp shock of what feels like electricity through their bodies during menopause. These shocks can feel odd and uncomfortable, even painful and can be linked to a hot flush.
The cause of ‘electric shock’ sensations during menopause isn’t completely understood. However, it’s thought to be a result of misfiring neurons in the brain related to lower levels of oestrogen which cause abnormal nerve sensations.
You are not alone if you feel drained and zapped of energy during the menopause – both physically and mentally.
During menopause, our hormone levels fluctuate dramatically which can disrupt sleep and leave us tossing and turning at night and waking up feeling unrefreshed.
Where insulin sensitivity is an issue, our cells don’t receive sufficient fuel from the food we eat which takes away our get-up-and-go. Thyroid issues, low iron levels and low B vitamins can also reduce energy levels
When we’re tired, we’re less likely to do exercise but this can set up a vicious circle as doing exercise boosts our energy.
Please note there are also medical conditions which can result in fatigue such as pain, sleep apnoea and infections – please discuss these with your doctor if you think they apply to you.

Do you think of yourself as having a sweet tooth? Do you often crave cake, biscuits and pastries, even if you’ve just eaten?
During menopause, many women experience more intense sugar cravings. You know these foods are unhealthy, but you feel you can’t stop yourself from eating them. There is some important biology behind these cravings – it’s not just about will power.
One factor is how effectively your body is able to use food for fuel (rather than storing it as fat). When our cells aren’t getting the fuel they need to function well, our body seeks out extra fuel (also known as chocolate!).
Another key factor is comfort eating. Sugary and flour based foods can cause a short term mood boost by increasing serotonin levels.
Oestrogen levels underpin these factors but rebalancing your insulin sensitivity and brain chemistry is key.
Thinning and lacklustre hair are common complaints during menopause. Women who once had thick, luscious, bouncy hair notice it’s become brittle, finer and prone to falling out. Hair loss is a natural part of ageing but can be exacerbated by menopause’s changing hormone levels.
Oestrogen is important in the hair growth cycle. When levels drop, hair is impacted not only by less oestrogen but also by the relative increase in the level of androgens. This hormonal shift can lead to hair loss.
Impaired thyroid function can play a role here as can chronic stress. Nutritional deficiencies should also not be overlooked. Anaemia (low iron) and low protein diets can result in thinning hair.
Headaches and migraines can get worse or suddenly start through perimenopause.
They are often triggered by hormone fluctuations so, as levels of oestrogen and progesterone fluctuate, they can become more frequent and more severe.
Other contributing factors include stress, lack of sleep, low levels of serotonin (the happy hormone) and hot flushes.
Studies also show that, for some women, eating food or drinks high in histamine and tyramine can provoke a migraine. These include foods that are aged (e.g. cheese) or fermented (e.g. sauerkraut) and also wine and beer.
Heart palpitations, irregular heartbeats or a racing heart can all happen through menopause. They can occur hand-in-hand with a hot flush or on their own and they can make you feel anxious and light-headed.
Typically, they are as a result of lower levels of oestrogen which affect the heart rate and the nervous system.
Other triggers include stress, low blood sugar, alcohol and caffeine.
Burning mouth syndrome can give rise to feelings of heat or tingling in or around your mouth. It’s one of the more unusual symptoms of menopause but not as rare as you might think – one study showed it can affect up to 1/3 of women.
In your mouth, your mucus membranes contain sex hormone receptors so a reduction in oestrogen during menopause can contribute to these uncomfortable sensations.
A burning mouth is also a possible result of under-functioning thyroid, mouth infections, allergies and having low iron levels or B vitamins.
Hot flushes are one of the most well-known menopausal symptoms and one experienced by many (about 3/4 of us).
They are known as a vasomotor symptom and they occur due to a change in the temperature regulation in the brain. Basically, our brain ‘over-reacts’ to a relatively small increase in temperature and we experience heat and can turn red and get sweaty.
The severity of hot flushes varies – about 30% of women experience extreme hot flushes – as does their frequency.
Oestrogen plays a big part here, but studies show that changes in blood sugar levels are also important. Women with diabetes or blood sugar problems suffer more with hot flushes.
Watch out for triggers that set hot flushes off. They commonly include caffeine, alcohol, hot drinks, spicy foods and hot baths & showers.
Unfortunately, hot flushes can persist long after menopause if underlying health issues persist. 40% of 60-65 year olds report still experiencing them.
In a recent study 70% of women felt that irritability was a problematic symptom of menopause. You may be suddenly less patient and quick to get cross. For some women, irritability disrupts their lives so badly that it warrants treatment.
There are a number of reasons why we can feel irritable. Hormonal imbalances, including oestrogen and cortisol levels, are key factors. And, of course, our day-to-day life plays a part – how much we have on, stress, how well we’ve eaten and our blood sugar levels (ever heard of feeling ‘hangry’?!) and lack of sleep to name but a few.
Women can experience anything from slightly to intensely itchy skin during menopause. These itchy sensations can occur particularly on your breasts, scalp and genitals.
This sensation is linked to drier skin (thanks to reduced sebum production linked to lower levels of progesterone) and reduced collagen (caused by falling oestrogen levels).
Together these make our skin more sensitive and less elastic. Dietary changes can improve collagen production and help skin stay hydrated.
If having sex is the last thing you’re up for, you’re not alone – up to half of menopausal women feel this way.
There are two interconnected elements that help us understand a drop in libido. First is desire which is controlled by the brain. Second is arousal – our body’s response to the idea of sex.
Reasons for no longer feeling desire include fatigue, low mood, stress, a decline self-confidence and the breakdown in a relationship.
Reasons for a drop in arousal include changes to blood supply and vaginal dryness which can make sex anything between underwhelming through to painful.
Changes in the levels of our sex hormones are key here – particularly oestrogen and testosterone. But our brain chemistry, iron levels, pelvic floor health, sleep patterns and exercise approach are important too.
Although menopause is linked to many physical symptoms, for some women it can have a huge impact on their mental health too. About half of women experience symptoms which include low mood, feelings of sadness and generally losing interest in life. Menopause is often misdiagnosed as depression because of the similarities in symptoms. In fact, for this reason, some doctors prescribe antidepressants vs other treatments.
Depression can be linked to fatigue, poor concentration, disrupted sleep, low sex drive, feelings of guilt or worthlessness and changes in appetite.
Lower levels of oestrogen are a factor here – because of the impact on levels of serotonin (the happy hormone). Stress and imbalanced cortisol levels can also leave you feeling unhappy.
Some women’s brains are more sensitive to changing hormone levels. If you suffered from post-natal depression or get PMS, you may notice a change in your mood through menopause.
Your memory seems like it’s playing tricks on you. Where are your keys, why did you walk into the kitchen and, sorry, what’s your name?
Memory lapses are common at menopause and are more likely to be linked to hormonal changes than early dementia.
Memory is a complex cognitive function that involves multiple parts of the brain working together. When oestrogen levels drop (or fluctuate up and down) it can affect your brain function and memory.
Other common factors are blood sugar and insulin sensitivity issues, stress and lack of sleep. For some women slow thyroid hormone function can make things worse.
Memory problems can be difficult to unravel but once you know what’s causing yours making changes makes a real difference.
Studies show lower levels of oestrogen can reduce serotonin levels which in turn can increase irritability, anxiety, anger, low mood and depression.
You might feel tearful and irrational one minute and then oddly OK the next. If you are still having periods, PMS can be much tougher.
Lower levels of progesterone, as a result of not ovulating, can leave you feeling overwhelmed and more tempted to eat or drink alcohol to achieve a sense of calm.
Finally, many women experience cortisol imbalances that can lead to angry or tearful outbursts.
Night sweats – or hot flushes at night – can be particularly hard to handle as they rob us of our sleep.
A night sweat can cause you to wake up drenched in sweat and needing fresh night clothes or even bed sheets. They happen for the same reasons as hot flushes.
Practical tips to handling night sweats include reducing the temperature of your room and having a thin duvet. Being overweight can increase the likelihood of night sweats and it’s best to avoid alcohol and smoking.
More significant is getting to the bottom of what’s causing these sweats which could include low levels of oestrogen, brain chemistry imbalances and blood sugar or insulin sensitivity issues.
Poor sleep can come in many forms. Perhaps it’s finding it hard to fall asleep or waking in the night and being unable to get back to sleep. It could be that you’re very restless or wake feel unrefreshed despite hours in bed.
A disrupted night’s sleep can leave you exhausted with a major knock-on effect on your physical and mental health the next day. According to the National Sleep Foundation, around 61% of menopausal women have sleep problems.
There are many reasons why we experience poor sleep. Commonly they are caused by night sweats, an over-active brain, needing to get up to go to the loo, snoring, blood sugar imbalances and high levels of cortisol.
You don’t need 8 hours every night but if you’re regularly sleeping less than 6 hours – prioritise your sleep.
Top tips – avoid stimulants (caffeine and smoking), reduce alcohol and keep your bedroom cool, dark and uncluttered.
Many of us are used to having sore breasts at some point in the second half of our menstrual cycle. This can get worse through perimenopause with breasts feeling anything from tender and uncomfortable through to experiencing stabbing pain.
Breast tissue is sensitive to hormones with discomfort occurring as oestrogen and progesterone levels fluctuate up and down.
As these hormones stabilise post menopause, most women find these sensations disappear. A low inflammatory diet can also make a huge difference.
One of the more unusual and unexpected symptoms of menopause is gum and dental problems. You may experience inflamed and bleeding gums, loose teeth, cavities, mouth tenderness, bad breath and infections.
Lower levels of oestrogen can reduce saliva production. This can increase your risk of tooth decay and gum disease because there isn’t sufficient saliva to rinse away oral germs and bacteria.
Oestrogen is also important for bone health – weaker bone structure in your jaw can result in wobbly teeth.
Supporting bones with adequate vitamin D, a nutrient dense diet and maintaining your dental hygiene will keep the tooth fairy happy.

As we age, many of us find our joints can become stiff, sore and painful. It could be that first 10 minutes after getting out of bed or walking down the stairs.
The most common areas for discomfort are the ‘high-impact’ joints such as hips and knees. The elbows, neck, shoulders, hands and fingers may also be affected.
Falling oestrogen levels can slow cartilage and bone formation. Your diet can pick up the slack if it’s packed with protein and minerals. Weight bearing exercise and flexing the joints can help too.
Tingling and pins & needles sensations in our legs, arms and hands are common menopause symptoms. Other sensations such as numbness, increased sensitivity and even the feeling of insects crawling on your skin (official name – formication) can occur.
One of the reasons behind these sensations is that fluctuating oestrogen levels can affect our central nervous system, but thyroid problems and inflammation can also contribute to these symptoms.
Urinary incontinence affects 1/3 of women in middle age. It is very common and not something to be embarrassed about.
To start with leaking, there are 2 main forms – stress incontinence (e.g. when you cough, sneeze or do exercise) and urge incontinence (when you urgently need to go to the loo and can’t hold it in).
You may be passing urine more frequently too, even waking in the night to visit the loo.
Lower levels of oestrogen impact the soft tissues throughout your body including in your bladder. Less oestrogen can cause your bladder to get irritated and want to empty before it’s full.
Factor in the strength of your pelvic floor as well. Weaker muscles (which can be exacerbated by excess weight) are less able to keep urine in your bladder.
Blood sugar problems also increase the need to urinate.
During and after menopause it’s common for women to suffer from pelvic health issues.
Vaginal dryness is linked to the natural decline of oestrogen which leads to vaginal atrophy meaning the vaginal walls become thinner and more easily irritated. In a survey, 1/3 of women reported experiencing vaginal dryness linked to menopause.
These changes can make anything from passing urine to intercourse uncomfortable. Lubricants can help and topical oestrogen can be prescribed even if you are not on or don’t want to use HRT.
Vaginal infections are more likely as a result of changes in our vaginal microbiome making the vagina less acidic. This creates an environment where it is easier for infections to take hold.
When it comes to bones, preventing a problem is the name of the game. Bones become weaker over a period of years so this is unlikely to be a symptom you experience through perimenopause or immediately after menopause.
Over time, however, bones lose density and are more likely to break – at a certain point this is diagnosed as osteoporosis. Approximately 1/3 of women will experience an osteoporosis related bone break in their lifetime.
More women than men suffer from osteoporosis because of the critical role oestrogen plays in bone health and specifically rebuilding bones. Lower levels of oestrogen means less renewal and less dense bones.
Calcium (a building block of bones) is important, as is vitamin D which is needed to absorb calcium and collagen which helps give bones their flexibility or ‘give’.
Weak bones can also be linked to having a low body weight, excess alcohol, smoking and certain genetics.
Lots of menopausal women put on weight or find it much harder to lose weight despite exercising harder and eating less. In fact, one study revealed that the average woman puts on 0.5kg per year from their mid 40s.
Menopausal weight gain is different from the weight gain you experienced when you were younger. It’s about an imbalance in ‘hunger hormones’ and a shift that that means you are more likely store food as fat.
Many women struggle with insulin resistance which is compounded by stress which also interferes with blood sugar. These encourage fat to be stored around the stomach, in particular.
Other factors include reduced muscle mass (muscles burn calories, even at rest), a slow thyroid impacting your metabolic rate and, last but not least, poor sleep.
Weight loss is much easier when your diet and supplements are focused on rebalancing your hunger hormones and managing cravings alongside doing the right type of exercise, improving how your body responds to stress and getting good quality sleep.
If you are frustrated and feeling self-conscious about weight you can’t shift, no matter what you try, check out our Lose Weight programme. We will create you a personalised plan that enables you to lose menopausal weight without feeling hungry and deprived.
Stay up to date with the latest menopause news by signing up to our mailing list
Newsletter Sign-up (popup)
Stay up to date with the latest menopause news